By Dave Dahl
SPRINGFIELD– Doctors and patients say they’ve had it with some paper-pusher at an insurance company standing between you and your treatment.
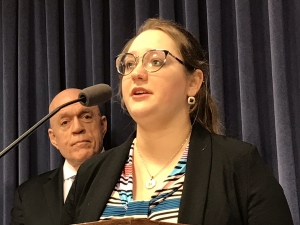
The Illinois State Medical Society brought Isabella McKenna to a Capitol news conference. She has dealt with severe arthritis for much of her life.
I had spent weeks unable to walk, weeks in horrible pain, yet unable to receive treatment, all because I could not get prior authorization from my insurance company in a reasonable time frame,” McKenna told reporters. “My father had to make countless phone calls, my doctor had to take the time to give them reason after reason why I needed this test.
“In the end, they — the insurance company, not my doctor — decided it was unnecessary.”
“As somebody who has been diagnosed with MS for over thirty years now,” said sponsoring State Sen. Linda Holmes (D-Aurora), “I understand the need for getting the authorized medical care that your physician — not someone who is reviewing documents (and) who doesn’t have this medical knowledge — has prescribed and said you need to maintain your best possible health.”
The bill, among other things, requires disclosure (such as on the insurer’s web site) about authorization policies; outlaws repeated requests for authorization of the same prescription drug; and requires comprehensive reviews — for example, approving both the anesthesia and the surgery.






